Foam-related challenges are common throughout oil and gas operations, from drilling and cementing to production and refining. Surfactants in drilling fluids, high agitation in mixing systems, and gas entrainment during circulation often create persistent foam. If unmanaged, foam can reduce mud density, disrupt pump efficiency, and interfere with solids control equipment—ultimately increasing operational costs and safety risks.

Modern oilfield operations require defoamers that perform under demanding conditions. Silicone, polyether, and specialized non-silicone formulations are used to rapidly break surface foam and prevent reformation under shear. Compatibility with high temperatures, salinity, and complex fluid chemistries is also critical. A well-selected defoamer helps maintain fluid integrity, improves separation efficiency, and supports smoother production and refining processes.
Rickman defoamer solutions are engineered for oil and gas applications, offering fast response and long-lasting suppression across drilling muds, cement slurries, fracturing fluids, and amine systems. Our team provides technical support, sample evaluation, and tailored recommendations based on real operational environments. Beyond product supply, Rickman works closely with partners to optimize performance, reduce chemical consumption, and improve operational reliability from wellsite to processing plant.
Click on the related products links:RK-30C(Excellent Stability Water-Based Defoamer) /RK-700P(High Effective Fermentation Antifoam)
How to Optimize Paper Mill Stability A Guide to Defoamer Applications
Foam formation is a common challenge in the paper industry, especially during pulping, stock preparation, and wet-end operations. High levels of surfactants from recycled fibers, sizing agents, and process chemicals often lead to persistent foam, which can affect drainage, sheet formation, and overall machine efficiency. Without proper control, foam may cause overflow, reduced production speed, and quality defects in finished paper.
Rickman defoamer solutions are developed with these real operating conditions in mind. Beyond supplying a wide range of defoamer chemistries, Rickman works closely with paper mills to evaluate process parameters, recommend suitable formulations, and adjust products based on on-site feedback. With stable supply capability, technical support, and application-driven service, Rickman helps paper producers achieve consistent foam control and smoother long-term operations.
Click on the related products links:RK-50P(Highly Efficient Polyether Ester Antifoam)/RK-203(Mineral Oil-based Defoamer)
FAQ
Q1: How do I choose between silicone and polyether defoamers for my paper mill?
A: Selection depends on the specific process stage. Silicone defoamers are ideal for pulp washing and high-shear areas due to their rapid foam-breaking speed. Polyether defoamers are better suited for the wet-end and fine paper production, as they offer excellent compatibility with sizing agents and won't cause "oil spots" on the finished sheet.
A: While dosage varies by system load, a common starting point for high-efficiency polyether-based defoamers is approximately 0.05% of the total flow. We recommend conducting a jar test to optimize the dosage based on your specific surfactant levels.
A: When used correctly, high-quality defoamers like Rickman’s formulations are designed to have minimal impact. In fact, by removing entrapped air, they often improve drainage and sheet formation, which can indirectly enhance the physical strength properties of the paper.
A: Yes. Rickman offers specialized silicone-based and mineral oil-based defoamers that maintain stability and efficacy even in high-temperature and high-alkali pulping environments, ensuring continuous process stability.

Different defoamer types serve different needs in papermaking. Silicone defoamers typically offer fast knockdown and strong persistence, making them suitable for high-temperature or high-shear systems. Polyether defoamers, on the other hand, are valued for their compatibility with sizing agents and minimal impact on paper appearance, especially in fine paper and tissue production. Selecting the right defoamer requires balancing foam control efficiency with system compatibility and final product requirements.
Q2: What is the recommended dosage of defoamer in white water systems?
Q3: Can defoamers affect the sizing efficiency or paper strength?
Q4: Are Rickman defoamers stable in high-temperature pulping processes?
Why Are Defoamers Critical in Oil and Gas Operations?
Foam-related issues are a persistent challenge across the oil and gas industry, from upstream drilling and production to midstream processing and wastewater treatment. Foam can disrupt separation efficiency, reduce throughput, increase chemical consumption, and even trigger safety risks during high-pressure operations. As production conditions become more complex, the role of a well-matched defoamer becomes increasingly important for stable and efficient operations.

Key Defoamer Application Scenarios in the Oil & Gas Industry
Different processes generate foam for different reasons, and defoamer selection must align with actual operating conditions rather than relying on a one-size-fits-all solution.
Application Area
Foam Source
Recommended Defoamer Type
Crude oil separation
Natural surfactants, gas entrainment
Silicone-based defoamer
Drilling fluids
Polymers, surfactants, high shear
Polyether-based defoamer
Produced water treatment
Oil residues, chemical additives
Compound defoamer
Refinery wastewater
Detergents, emulsified oil
Silicone or hybrid defoamer
In produced water treatment systems, for example, adding 0.03–0.08% of a properly selected defoamer can significantly reduce surface foam during continuous operation, helping maintain separator efficiency without affecting downstream treatment performance.
Silicone vs. Polyether Defoamers: Which Works Better in Oil & Gas?
Understanding the differences between defoamer chemistries helps operators make more reliable choices under demanding conditions.
-
Strong and fast foam knockdown
-
High resistance to temperature and salinity
-
Suitable for crude oil processing and high-load wastewater systems
-
Better dispersion in aqueous systems
-
Lower risk of oil-water separation interference
-
Commonly used in drilling fluids and circulation systems
In high-temperature separators or gas-liquid separation units, silicone defoamers often deliver more consistent results. In contrast, polyether defoamers are preferred where compatibility with fluid systems and controlled foam suppression are critical.
Real Applications, Real Shipments: Rickman in Action
Rickman defoamers are currently supplied to oilfield service companies and wastewater operators across Asia, the Middle East, and Africa. In one recent application, a compound defoamer was delivered for a produced water treatment facility handling high oil content and fluctuating flow rates. On-site feedback confirmed stable foam control over multiple operating cycles, with no negative impact on oil-water separation efficiency.
Each shipment is prepared according to customer specifications, including packaging type, labeling, and logistics requirements. From bulk IBC containers to customized drums, Rickman ensures products arrive ready for immediate use under field conditions.
Why Oil & Gas Clients Choose Rickman Defoamer
Beyond product performance, Rickman places strong emphasis on service and long-term cooperation. Our technical team works closely with customers to evaluate system parameters such as temperature, salinity, shear force, and chemical compatibility before recommending a solution. Sample testing, formulation adjustment, and post-delivery support are all part of Rickman’s service approach, helping customers reduce trial-and-error costs and improve operational reliability.

FAQ
Q1: How do I select the right defoamer for oil and gas applications?
A: Selection should be based on process conditions such as temperature, salinity, shear force, and foam persistence. Field testing and technical evaluation are strongly recommended before large-scale use.
Q2: Are silicone defoamers always better for oil and gas systems?
A: Not necessarily. While silicone defoamers offer strong knockdown performance, polyether or compound defoamers may be more suitable for certain drilling fluids or wastewater systems where compatibility is critical.
Q3: Can Rickman provide customized defoamer solutions for oilfields?
A: Yes. Rickmanoffers application-specific formulation adjustments and technical support to match different oilfield conditions and operational requirements.
Why Is Defoamer Essential in the Paint Industry?
In the paint industry, foam formation is a major concern that can disrupt production and degrade product quality. Whether it is during the mixing process, application, or storage, foam can cause inconsistencies in paint viscosity, poor surface finish, and even equipment malfunctions. That’s why choosing the right defoamer is essential to maintain high-quality paint production and optimize efficiency. But with various options available, how do you know which defoamer is the best fit for your system?

Comparing Defoamers for Paint Production: Silicone vs. Polyether-Based Solutions
There are several types of defoamers used in paint production, but two of the most common categories are silicone-based defoamers and polyether-based defoamers. Understanding the differences between these two types can help you select the best solution based on your paint formulation and processing conditions.
Silicone-Based Defoamers: Quick Action, High Stability
Silicone defoamers are typically known for their rapid foam-breaking properties and high stability in harsh environments, including high temperature and shear conditions. They are commonly used in solvent-based and high-viscosity paints.Advantages:
- Fast Foam Knockdown: Quickly breaks foam upon application.
- High Temperature Tolerance: Performs well under higher temperatures.
- Durable: Provides long-lasting suppression.
Best Applications:
- High-gloss coatings
- Solvent-based paints
- Industrial coatings

Polyether-based defoamers, on the other hand, are known for their cost-effectiveness and compatibility with water-based paints. They work well in formulations that require minimal impact on the paint’s appearance and texture.
- Cost-effective: Less expensive compared to silicone defoamers.
- Low Impact on Surface Properties: Does not affect gloss or surface quality.
- Suitable for Water-Based Paints: Performs well in emulsions and waterborne systems.
- Water-based paints
- Architectural coatings
- Decorative finishes
Comparison of Silicone vs. Polyether-Based Defoamers
Property
Silicone-Based Defoamer
Polyether-Based Defoamer
Speed of Action
Fast foam break
Moderate foam suppression
Temperature Tolerance
High tolerance to heat
Moderate, sensitive to heat
Cost
Higher cost
More economical
Impact on Surface Quality
May affect gloss and texture
Minimal impact on gloss and texture
Better for
Solvent-based and industrial paints
Water-based paints and emulsions
Why Choose Rickman Defoamer for Your Paint Production?
Rickman’s defoamer solutions are designed with the specific needs of the paint industry in mind. We offer both silicone and polyether-based defoamers, providing versatile solutions that cater to different production environments. Our defoamers are formulated to provide optimal foam control, reduce production time, and improve overall product quality, ensuring that your paints maintain their desired properties throughout the manufacturing process.

FAQ
Q1: What is the difference between silicone and polyether-based defoamers?
A1: Silicone-based defoamers are typically faster-acting and more stable at higher temperatures, making them ideal for solvent-based and industrial coatings. Polyether-based defoamers, on the other hand, are more economical and work well in water-based paints, offering minimal impact on surface quality.
Q2: How do I know which defoamer to choose for my paint formulation?
A2: The choice of defoamer depends on factors such as the type of paint (solvent-based or water-based), the production process, and the desired finish. Silicone defoamers are ideal for high-viscosity and solvent-based paints, while polyether defoamers are more suitable for water-based formulations.
Q3: Can Rickman help me optimize foam control in my paint production?
A3: Yes! Rickman offers personalized solutions and technical support to ensure the most effective foam control for your paint formulations, optimizing production efficiency and product quality.
A Comparison of Fixed-Speed vs. Inverter Water Pressure Booster Pumps
Many households face the frustration of low water pressure. Whether you live on the top floor of a high-rise or in a standard residential community, common issues include weak shower flow, inefficient toilet flushing, and slow-filling washing machines.
To meet this demand, the market offers two primary solutions: traditional fixed-speed and modern inverter (variable-frequency) pressure booster pumps. This analysis compares their technology, application, cost-effectiveness, and performance to help you make an informed, scientific decision.
Core Technology & Key Differences is the fundamental difference lies in motor control:
1. Fixed-Speed Pumps use standard asynchronous motors that start via direct-on-line or star-delta methods. They operate at a constant speed (typically 2850 RPM), delivering fixed power output. This means the pump always runs at its maximum head and flow rate, unable to adjust to actual water demand.
2. Inverter (Variable-Frequency) Pumps integrate an intelligent control system. Key components include a Variable Frequency Drive (VFD), pressure sensors, and a PID controller. The system continuously monitors pipeline pressure via sensors. This data is processed by the PID controller, which instructs the VFD to adjust the motor's input frequency (typically within 0-50Hz/60Hz range), enabling seamless speed variation. This closed-loop control ensures pump output precisely matches real-time water consumption.
Performance Comparison:
1. Pressure Stability
Fixed-Speed Pumps exhibit significant pressure fluctuation. Opening multiple water points causes a pressure drop, while reduced flow can lead to pressure spikes. Although some advanced models include a pressure tank for buffering (usually 8-24L), pressure swings can still reach 10-20%.
Inverter Pumps maintain remarkably constant pressure. For example, MASTER EAGLE inverter pumps keep pressure variation within ±2%, even as flow changes from zero to rated capacity. This is crucial for appliances requiring stable pressure.
2. Energy Efficiency
Fixed-Speed Pumps are inefficient at partial load. Even at 30% of rated flow, they consume near-full power. Frequent start-stop cycles, each drawing 2-3 times the rated current, further increase energy costs.
Inverter Pumps adjust output to demand, typically saving 30-50% in energy consumption. Third-party tests show that for an annual water use of 120 cubic meters, an inverter pump can save about 280 kWh. At a residential rate of $0.09/kWh, this translates to approximately $25 in annual savings.
3. Noise & Lifespan
Fixed-Speed Pumps generate noticeable vibration and noise (65-75 dB, similar to city traffic), especially during the high-current startup shock, which stresses components like bearings and impellers.
Inverter Pumps utilize soft-start technology for smooth acceleration, drastically reducing mechanical wear and noise (50-60 dB, akin to normal conversation). For instance, MASTER EAGLE smart inverter pumps demonstrate a bearing life 2.3 times longer and impeller life about 40% greater than fixed-speed models.
Ideal Application Scenarios:
Fixed-Speed Pumps Are Suited For:
1. Temporary/Short-Term Use: Rentals, construction sites where low upfront cost and simple maintenance are priorities.
2. Single-Point Applications: Boosting pressure for an isolated bathroom or outdoor faucet with consistent, simple demand.
3. Tight Budgets: A viable basic solution for cost-conscious homeowners.
Inverter Pumps Are Recommended For:
1. Whole-House Systems: Villas, multi-story homes with simultaneous demand from showers, appliances, etc., requiring dynamic balancing.
2. Pressure-Sensitive Appliances: Protecting devices like gas water heaters, wall-hung boilers, or smart toilets from damage due to pressure fluctuations.
3. Long-Term Energy Savings: For users with daily consumption over 0.5 cubic meters and annual operation exceeding 2000 hours, the higher initial investment can be recouped via electricity savings within 2-3 years.
Key Purchase Considerations:
1. Initial Investment
Fixed-speed pumps range from $30-$100, while inverter pumps typically cost $120-$350. For example, a 150W fixed-speed model might cost $85, versus $275 for a 250W inverter model—a $190 difference. Based on annual energy savings of $25, the payback period is roughly 7.6 years, potentially shortening to 5-6 years when considering extended equipment lifespan and replacement cost avoidance.
2. Installation & Maintenance
Fixed-Speed: Simple installation (connect pipes and power). Maintenance involves checking pressure tank air pre-charge (0.1-0.15 MPa) every 6 months and replacing seals every 2 years (~$7 annual cost).
Inverter: Requires professional installation for parameter setup (pressure set-point, acceleration time). Maintenance includes quarterly cleaning of the VFD cooling fan and annual sensor calibration (~$20 annual cost). VFD repair can cost $75-$120.
Integrated Solutions:
High-Rise Building Water Supply: For buildings over 20 floors, an inverter pump system can provide intelligent boosting. A main pump (30m head) in the basement, linked via IoT to a rooftop tank level gauge, ensures automatic refilling with minimal pressure fluctuation (<0.02 MPa).
Rural Decentralized Water Supply: In areas without centralized systems, an inverter pump paired with a water tower or tank (e.g., 5 cubic meters) ensures 24/7 supply while preventing water hammer caused by frequent pump cycling.
Solar/Heat Pump Water Heater Systems: These require extreme pressure stability. An inverter pump with constant-pressure function minimizes temperature stratification, reducing startup temperature swing from ±5°C to within ±1°C.
Future Trends & Innovations:
The market is evolving towards smarter inverter pumps. High-end models now feature APP remote control, water usage monitoring, and fault alarm. Users can set time-based pressure modes (e.g., lower at night), and systems auto-optimize based on usage history.
In material science, Permanent Magnet Synchronous Motor (PMSM) technology is boosting efficiency further. Fuzhou Mastere Eagle Electrics Co.,Ltd provide the PMSM inverter pumps achieve 15-20% higher efficiency than traditional asynchronous motor models, with a 30% smaller footprint and noise levels below 45 dB.
For most homeowners with sufficient budget and long-term plans (over 5 years), an inverter pressure booster pump is the better choice. The benefits in stable pressure, energy savings, and extended equipment life significantly enhance water experience and reduce total cost of ownership. For temporary needs or extremely tight budgets, a fixed-speed pump remains a functional basic solution. Your final decision should balance specific application scenarios, financial considerations, and desired quality of life.
If you would like to learn more, please visit our website: www.fzwatersystem.com
Beyond Basic Safety Why LFGB Certification is the "Gold Standard" for Water Pumps
When sourcing components for fluid handling—whether for a high-end coffee machine, a medical device, or a smart water dispenser—engineers and buyers often check one box: "Food Grade."
Usually, this means the product meets FDA (US) standards. While FDA compliance is essential, it is not the ceiling of safety; it is the floor.
At [Your Company Name], we operate by a stricter benchmark: the German LFGB standard. Today, we are pulling back the curtain on why this certification matters for water pumps and why it is the defining factor between a "safe" pump and a "premium" one.
What Exactly is LFGB?
LFGB stands for Lebensmittel-, Bedarfsgegenstände- und Futtermittelgesetzbuch (German Food, Consumer Goods and Feed Code). It is Europe’s toughest legal framework for managing food hygiene.
Any material that comes into contact with food—or in our case, water and beverages—must pass rigorous testing under Sections 30 and 31 of the LFGB.
While the "Knife and Fork" symbol is common on Tupperware, for water pumps, this certification is about the internal components: the valve heads, the diaphragms, and the plastic chambers that the fluid travels through.
The Hidden Danger in Pumps: Why Testing Matters
You might wonder, “It’s just a pump. Why is the testing so strict?”
Water pumps, specifically micro-diaphragm pumps, rely on soft, flexible materials (like silicone, EPDM, or TPV) to create pressure.
- Chemical Migration: Under high pressure or high temperatures (like in an espresso machine), inferior rubber or plastic can break down, leaching chemical compounds into the water.
-
Sensory Impact: Have you ever drunk water from a dispenser that tasted like "plastic" or "rubber"? That is the result of volatile organic compounds (VOCs) releasing from non-compliant pump materials.
LFGB vs. FDA: The Battle for Quality
This is the most common question we receive from our B2B clients: "Is FDA good enough, or do I need LFGB?"
To answer this, we must look at how they are tested.
1. The FDA Approach (The Composition Check)
FDA testing generally focuses on the raw material ingredients. If the silicone used in the pump diaphragm is made from an "approved list" of ingredients, it is typically deemed compliant. It is a safety check.
2. The LFGB Approach (The Performance Check)
LFGB goes much deeper. It focuses on Migration Testing. Labs simulate real-world conditions using different solvents (simulating water, acid, alcohol, and fat) to see if anything transfers from the pump material to the liquid.
3. The "Sensory Test" (The Dealbreaker)
This is where LFGB distinguishes itself. It includes rigorous Organoleptic (Sensory) Testing. Even if a pump is chemically safe, if it imparts any detectable smell or taste to the water, it fails LFGB testing.
Expert Insight: For coffee machine manufacturers, the Sensory Test is non-negotiable. The perfect espresso requires pure water. An FDA-compliant pump might still ruin the coffee's flavor profile with a rubbery aftertaste. An LFGB-compliant pump will not.
| Feature | FDA Standard (USA) | LFGB Standard (Germany/EU) |
| Focus | Ingredient safety | Chemical Migration + Sensory Experience |
| Strictness | Standard | High / Intensive |
| Cost of Material | Lower | Higher (Requires high-purity curing agents) |
| Best Application | General hydration | Premium coffee, tea, baby formula |
How We Engineer for LFGB Compliance
Achieving LFGB certification for a water pump isn't easy. It requires specific engineering choices that we have integrated into our manufacturing process:
-
Platinum-Cured Silicone: Unlike standard peroxide-cured silicone (which is cheaper but can smell), we use platinum-curing processes for our diaphragms. This ensures high tear resistance and zero odor.
-
High-Stability Plastics: Our pump housings use medical-grade plastics that withstand high temperatures without degrading or releasing micro-particles.
-
Third-Party Verification: We don't just say we are compliant. We submit our components to accredited testing agencies (such as TÜV Rheinland or SGS) to verify compliance with LFGB Sections 30 & 31.
Why This Matters for Your Business
If you are a manufacturer integrating our pumps into your devices, choosing LFGB components offers three distinct advantages:
-
Market Access: You cannot sell food-contact electronics in Germany or France without this standard. It opens the door to the entire EU market.
-
Brand Protection: It protects your brand from consumer complaints regarding "bad tasting water."
-
Durability: Materials that pass LFGB migration tests are inherently more stable. They last longer, meaning your pumps have a longer service life with fewer failures.
How the bottled water system working?
Portable Pump System for Dispensing Potable Water from Standard Water Bottles.
The BW5000 series bottled water system is designed to pump purified water from commercially available 5-gallon purified water bottles. The system will deliver the water under pressure to an individual drinking water faucet, the water inlet of a refrigerator for the ice-maker and chilled drinking water tap, to a faucet in portable sinks and to certain personal use and commercial use coffee / tea brewers / espresso machines.
When the suction wand is inserted into the standard 5-gallon bottle, it will activate the float switch on the end of the wand and turn on the pump. This same float switch shuts off the system when the bottle is empty. The wand has a built in back-flow prevents valve that prevents water in the system from flowing back into the bottle, or spilling while changing bottles. The heart of the system is the main module that automatically fills an appliance or dispenses water through a faucet when there is demand. The system is equipped with an automatic thermal cut-off device for additional protection.
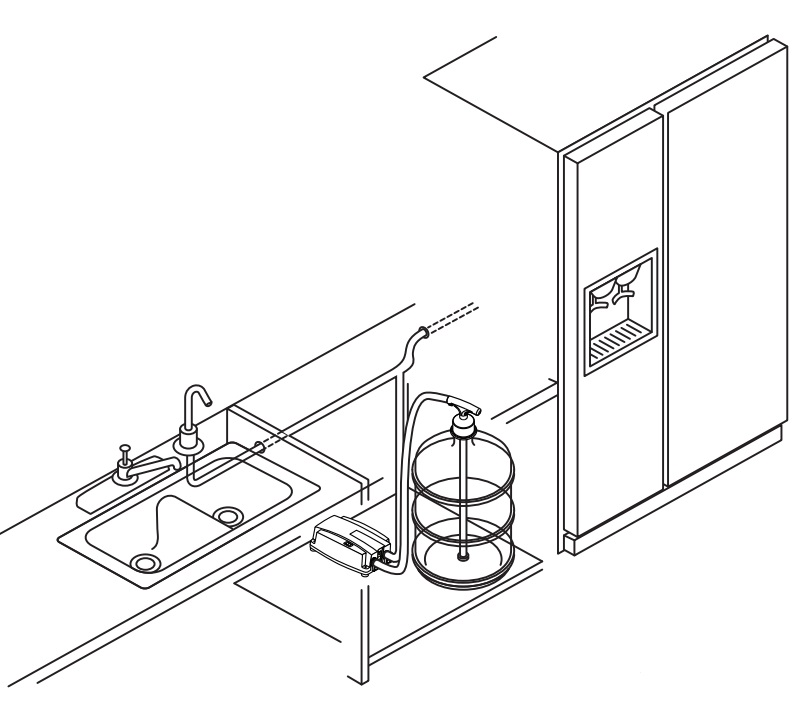
Select a cabinet large enough to accommodate the 5 gallon (19L) bottle and suction wand assembly. Place the pump module on the floor of the cabinet with on/off switch and suction tube facing out toward the cabinet doors. Position as close as possible to a grounded electrical outlet and place the five gallon bottle close to the pump module without kinking the suction hose
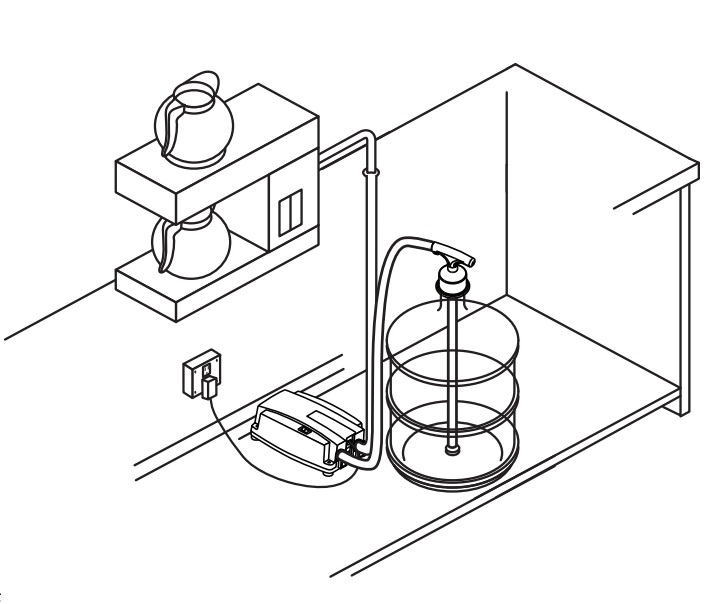
The bottled water dispensing system may also be placed in a pantry, closet, cellar or other location where a grounded electrical outlet is available.
MASTER EAGLE Reliable Intelligent Water & Energy Solutions Provider Since 2017
When it comes to sourcing durable, efficient water pumps and energy products for residential, commercial, or industrial use, global buyers increasingly turn to MASTER EAGLE. Founded in 2017 and based in Fuzhou, China’s maritime Silk Road hub with robust manufacturing ecosystems, we’ve spent over 8 years refining our craft, earning trust from clients across the Middle East, Africa, and Southeast Asia. Our journey isn’t just about selling products; it’s about solving real-world water and energy challenges with expertise honed through hands-on industry experience.
From Specialized Export to Integrated Manufacturing
Every great solution starts with understanding the market, and we’ve built our foundation on direct, on-the-ground experience. In 2017, we launched with a focus on exporting small-power generators, electric motors, and water pumps. Early on, we noticed a gap: buyers needed more than “standard” products—they needed tailored solutions for harsh climates (like desert heat in the Middle East) and remote areas (where grid power is unavailable in Africa).
To address this, we expanded beyond trading to build two owned manufacturing facilities and partner with three specialized factories in Fujian and Zhejiang (China’s top industrial provinces). This integration let us control every production stage, from raw material selection (we source 304 stainless steel for pump casings to resist corrosion) to final testing (each pump undergoes 48-hour pressure and efficiency checks). By 2020, our on-site engineering team had modified 12 product iterations based on client feedback, including a solar water pump design that boosts energy efficiency by 22% in low-light conditions. This hands-on experience ensures our products don’t just meet specs; they perform in the field.
Technical Depth in Water & Energy Solutions
- Intelligent Variable Frequency (VF) Water Pumps: Equipped with our self-developed VF controller, these pumps automatically adjust flow rate based on water demand—reducing energy consumption by up to 35% compared to fixed-speed models. We’ve optimized the controller’s heat dissipation system for temperatures up to 55°C, a critical upgrade for Middle Eastern clients. Our engineering team publishes case studies on this technology in industry journals like Water Technology.
- Solar-Powered Water Pumps: For off-grid areas, our solar pumps combine monocrystalline silicon panels (25% conversion efficiency) with brushless DC motors. We recently completed a project for a Kenyan rural community, installing 50 solar pumps that supply clean water to 1,200 households—eliminating their reliance on diesel generators. The system’s durability was validated by third-party testing: it operates continuously for 2,000+ hours without maintenance.
- Complete Bottled Water & Emergency Systems: We’ve extended our expertise to end-to-end solutions, including manual bottled water pumps (ideal for disaster relief) and automated filling systems for bottled water factories. A UAE-based bottled water brand increased production efficiency by 40% after switching to our custom filling system verified by their 2023 operational report.
Trusted by Partners & Certified for Quality
We hold ISO 9001 Quality Management System Certification, and our products meet CE (European Union) and SASO (Saudi Arabia) standards—essential credentials for global markets.
We provide full product traceability; every unit has a unique serial number linked to its raw material batch, production date, and test results, accessible via our client portal. Our quality guarantee isn’t just a slogan: we offer a 2-year warranty on all pumps (double the industry average) and have a dedicated after-sales team based in Dubai and Nairobi to resolve issues within 48 hours.
Why Choose MASTER
Whether you’re a distributor looking for reliable inventory, a construction firm needing durable pumps for remote sites, or a community organization sourcing solar water solutions, we bring three non-negotiables: experience-backed design (8+ years solving regional challenges), technical expertise (customizable solutions with verified efficiency), and proven trust (certifications, long-term partnerships, and client testimonials).
We’re not just a supplier; we're your long-term partner in navigating water and energy complexities. Contact our team today to request a product sample, access our technical white paper on solar pump efficiency, or discuss your specific project needs.
Smart Pump Technology Revolution 3 Breakthrough Solutions for Modern Water Systems
In the rapidly evolving water management industry, intelligent pumping systems have become game-changers for residential, agricultural, and industrial applications. This article explores three cutting-edge technologies transforming water delivery efficiency worldwide: intelligent inverter pumps, constant pressure water pumps, and variable frequency pumps.
1. Intelligent Inverter Pumps: The Brain of Modern Hydraulics
Our latest intelligent inverter pump series integrates IoT sensors and AI-driven control algorithms, achieving 40-60% energy savings compared to conventional models. These self-learning systems automatically adjust operations through:
- Real-time flow demand analysis via pressure transducers
- Motor speed optimization (200-4000 RPM range)
- Predictive maintenance alerts for shaft alignment/impeller wear
Key applications:
- Solar-powered irrigation systems
- Smart building HVAC networks
- Industrial coolant circulation
A recent Dubai hotel project reduced annual water costs by $28,500 using these pumps with photovoltaic integration.
2. Constant Pressure Water Pumps: Stability Redefined
Engineered for zero-pressure-fluctuation performance, our constant pressure water pumps maintain ±1.5 PSI precision through:
- PID-controlled permanent magnet motors
- Built-in expansion tank buffering
- Instantaneous flow compensation technology
- Performance highlights:
- 24/7 operation at 55dB noise level
- Dry-run protection with auto-shutdown
- Compatible with smart home systems (Zigbee/Modbus)
Ideal for:
High-rise building water supply
Automated farming irrigation
Fire suppression systems
3. Variable Frequency Pumps: Precision Meets Versatility
The variable frequency pump series combines VFD technology with hydraulic engineering breakthroughs:
0.5Hz frequency control resolution
7-inch HMI touchscreen interface
Energy efficiency class IE5
Technical advantages:
30% longer bearing lifespan through smooth start-stop
Multi-pump cascade control capability
Saltwater corrosion resistance (IP68 rating)
Case study: A California vineyard achieved a 22% yield increase using our solar-VFD pump system with soil moisture sync.
|
Comparative Analysis |
|||
|
Feature |
Inverter Pump |
Constant Pressure |
Variable Frequency |
|
Energy Saving |
40-60% |
25-35% |
35-50% |
|
Pressure Control |
±2 PSI |
±1.5 PSI |
±3 PSI |
|
Smart Connectivity |
WiFi/4G |
Zigbee |
Modbus/Profibus |
|
Typical ROI Period |
8-14 months |
12-18 months |
10-16 months |
The function and working principle of water pump frequency converter
A pump frequency converter is an electrical transmission component that controls AC motors by adjusting the frequency and amplitude of their power supply. For water pumps, its primary functions include optimizing three-phase AC motor startup methods and achieving smooth speed regulation.
Features of Water Pump Frequency Converters:
*Designed for constant-pressure energy-saving control,
*These converters integrate PID algorithms and advanced energy-saving software to Enable multi-point pressure timing functions with time-sharing operation per load.
*20% -60% energy savings (depending on actual conditions),
*Feature simplified management with safety protection and automated control,
*Extend equipment lifespan, stabilize power grids, reduce wear, and lower failure rates.
Operating Principles:
These converters can also regulate single-phase asynchronous motor speeds and receive two-phase current from capacitors.
Typically, they consist of a rectifier unit converting AC to DC and supplying power to DC intermediate circuits, along with an inverter that outputs voltage at specified frequencies and amplitudes. When driving AC motors, they provide sleepless acceleration from zero to rated speed without torque reduction. Due to strong electromagnetic interference generated on motor power lines, proper shielding is essential. Additionally, installing a sine wave filter between the pump converter and pipeline booster motor converts the converter's PWM output into a sinusoidal waveform.